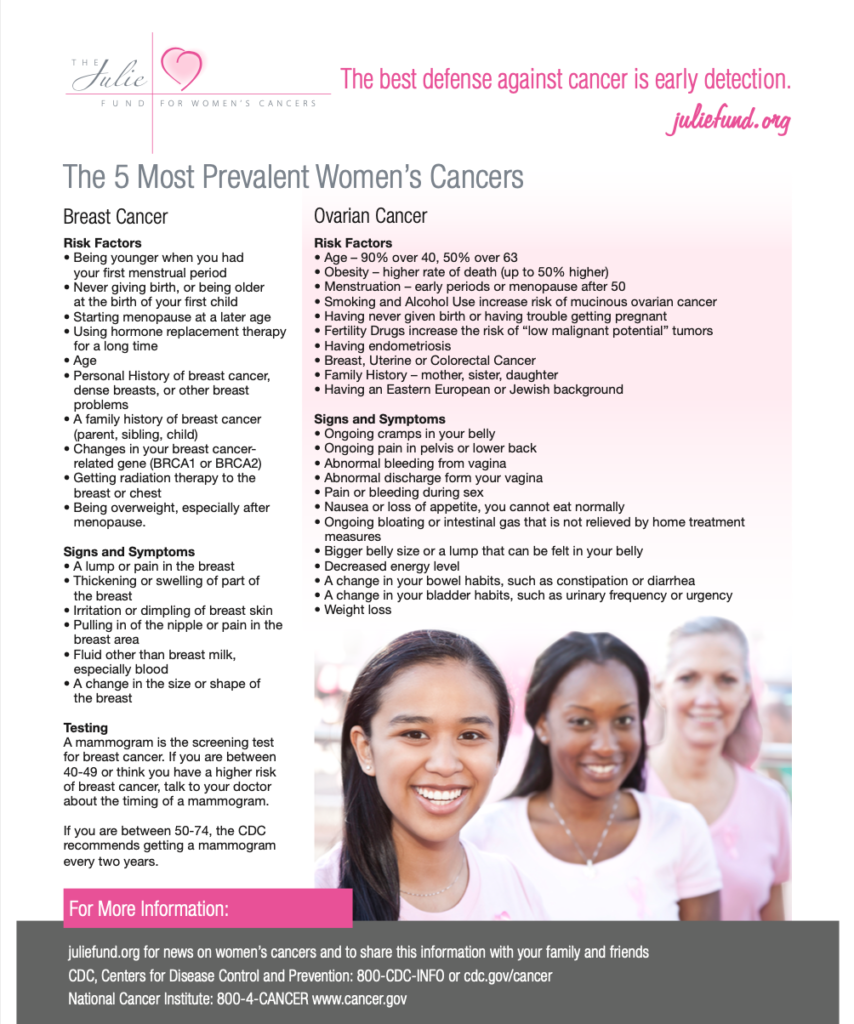
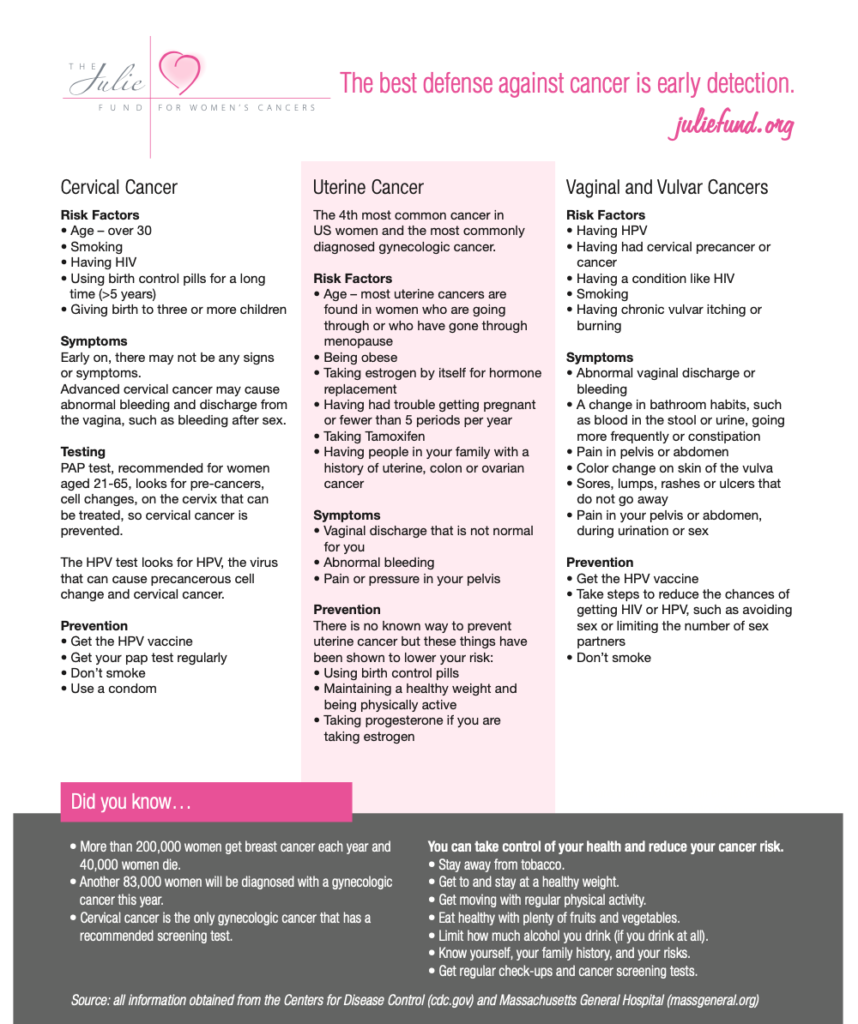
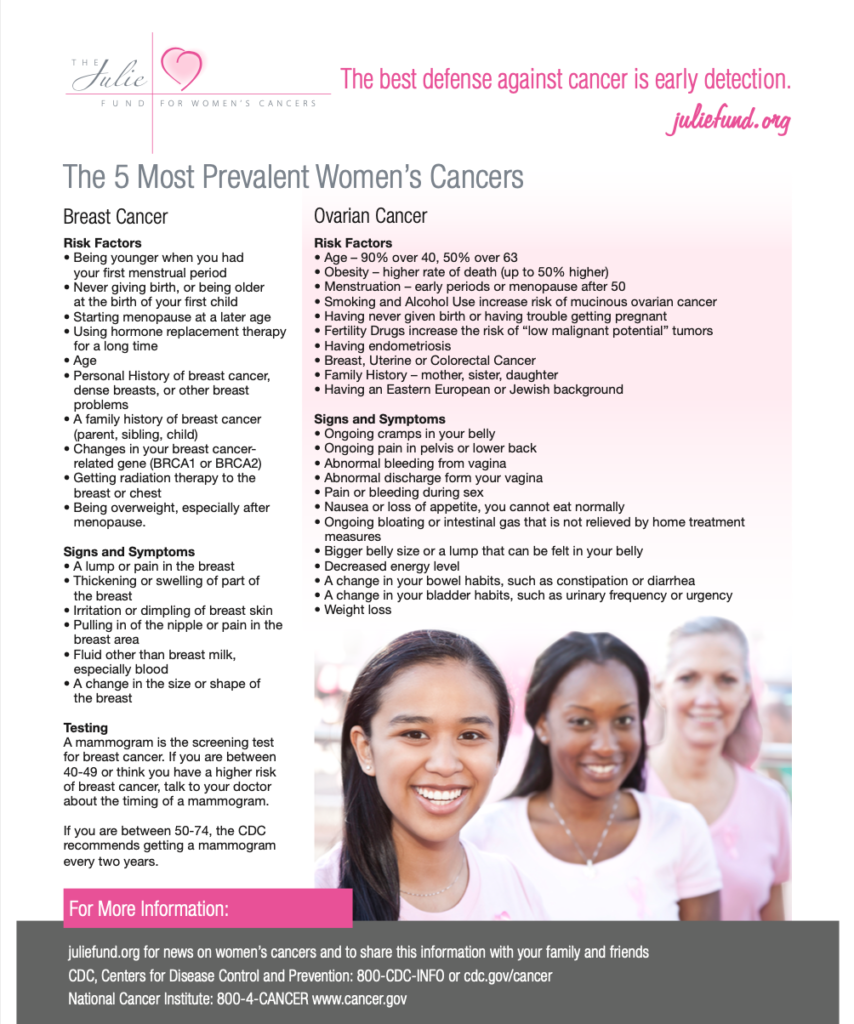
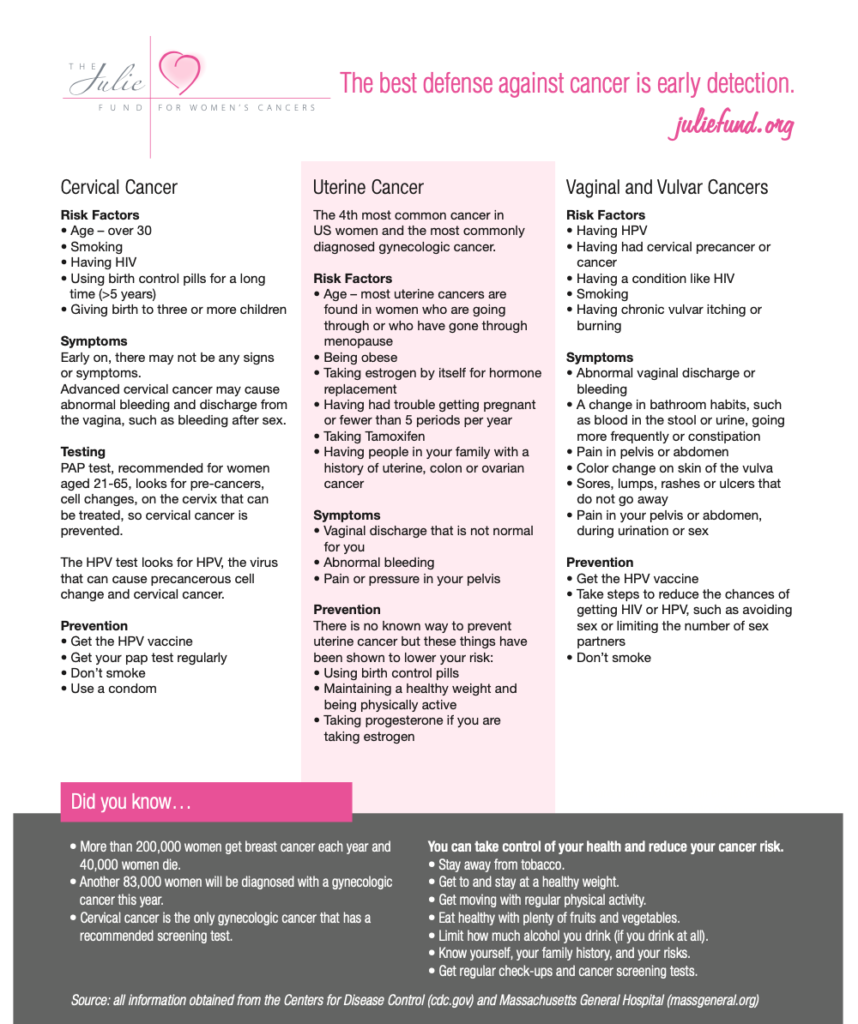
Early detection is the best defense against cancer. Please use this guide for risk factors and early warning signs.

for women's cancers
Early detection is the best defense against cancer. Please use this guide for risk factors and early warning signs.